2019–20 coronavirus (covid-19) pandemic and wikipedia
2019–20 coronavirus (covid-19) pandemic and wikipedia

The 2019–20 coronavirus pandemic is an ongoing pandemic of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS‑CoV‑2). The outbreak was identified in Wuhan, China, in December 2019.[4] The World Health Organization declared the outbreak a Public Health Emergency of International Concern on 30 January, and a pandemic on 11 March.[6][7] As of 28 April 2020, more than 3.08 million cases of COVID-19 have been reported in 185 countries and territories, resulting in more than 213,000 deaths. More than 915,000 people have recovered.[5]
The virus is primarily spread between people during close contact,[c] often via small droplets produced by coughing,[d] sneezing, or talking.[8][9][11] The droplets usually fall to the ground or onto surfaces rather than remaining in the air over long distances.[8][12][13] People may also become infected by touching a contaminated surface and then touching their face.[8][9] In experimental settings, the virus may survive on surfaces for up to 72 hours.[14][15][16] It is most contagious during the first three days after the onset of symptoms, although spread may be possible before symptoms appear and in later stages of the disease.[17]Common symptoms include fever, cough, fatigue, shortness of breath, and loss of smell.[8][18][19] Complications may include pneumonia and acute respiratory distress syndrome.[20] The time from exposure to onset of symptoms is typically around five days, but may range from two to fourteen days.[21][22] There is no known vaccine or specific antiviral treatment.[8] Primary treatment is symptomatic and supportive therapy.[23]
Recommended preventive measures include hand washing, covering one's mouth when coughing, maintaining distance from other people, wearing a face mask in public settings, and monitoring and self-isolation for people who suspect they are infected.[8][24] Authorities worldwide have responded by implementing travel restrictions, quarantines, curfews and stay-at-home orders, workplace hazard controls, and facility closures. Many organizations have also worked to increase testing capacity and trace contacts of infected persons.[citation needed] There is no evidence that recovered people are immune, and multiple patients have tested positive again after recovery.[25][26]
The pandemic has caused severe global socioeconomic disruption,[27] including the largest global recession since the Great Depression.[28] It has led to the postponement or cancellation of sporting, religious, political and cultural events,[29] widespread supply shortages exacerbated by panic buying,[30][31] and decreased emissions of pollutants and greenhouse gases.[32][33] Schools, universities and colleges are closed either on a nationwide or local basis in 194 countries, currently affecting approximately 98.5 per cent of the world's student population.[34] Misinformation about the virus has spread online,[35] and there have been incidents of xenophobia and discrimination against Chinese people and against those perceived as being Chinese, or as being from areas with high infection rates.[36][37][38]
STAY HOME.
SAVE LIVES.
Help stop coronavirus
1
STAYhome as much as you can
2
KEEPa safe distance
3
WASHhands often
4
COVERyour cough
5
SICK?Call aheadHealth authorities in Wuhan, Hubei, China, reported a cluster of pneumonia cases of unknown cause on 31 December 2019,[321][322] and an investigation was launched in early January 2020.[323] These cases mostly had links to the Huanan Seafood Wholesale Market and so the virus is thought to have a zoonotic origin.[324] The virus that caused the outbreak is known as SARS‑CoV‑2, a newly discovered virus closely related to bat coronaviruses,[325] pangolin coronaviruses,[326][327] and SARS-CoV.[328] The analysis of of SARS‑CoV‑2 RNA sequence found no evidence that the virus was made in a laboratory or engineered.[329][330]
According to the initial reports by Chinese government, the earliest known patient had onset of symptom on 8 December 2019, meaning that the first human infections took place in November 2019 because of the incubation period[331] The case had no visible connections with the later wet market cluster.[331][332] Of the early cluster of cases reported that month, two-thirds were found to have a link with the market.[333][334][335] On 13 March 2020, South China Morning Post reported that a 55-year-old from Hubei has been the first person to contract Covid-19 on 17 November 2019, and one to five new cases have been reported to Chinese government each day since then.[336][337]
Cases
Cases refers to the number of people who have been tested for COVID-19, and whose test has been confirmed positive according to official protocols.[338] As of 23 April, the countries that made public their testing data have on average performed a number of tests equal to only 1.3 per cent of their population, while no country has tested samples equal to more than 13.4 per cent of its population.[339] Many countries have had official policies to not test those with only mild symptoms.[340][341] An analysis of the early phase of the outbreak up to 23 January estimated 86 per cent of COVID-19 infections had not been detected, and that these undocumented infections were the source for 79 per cent of documented cases.[342] Several other studies, using a variety of methods, have estimated that numbers of infections in many countries are likely to be considerably greater than the reported cases.[343][344]
On 9 April 2020, preliminary results found that 15 per cent of people tested in Gangelt, the centre of a major infection cluster in Germany, tested positive for antibodies.[345] Screening for COVID-19 in pregnant women in New York City, and blood donors in the Netherlands, has also found a number of positive tests that may indicate infections may be higher than reported.[346][347] However, such antibody surveys can be unreliable due to a selection bias in who volunteers to take the tests, and due to false positives. Some results (such as the Gangelt study) have received substantial press coverage without first passing through peer review.[348]
Analysis by age in China indicates that a relatively low proportion of cases occur in individuals under 20.[349] However, it is not yet clear whether this is because young people are actually less likely to be infected, or less likely to develop serious symptoms, and thus seek medical attention and be tested.[350]
Initial estimates of the basic reproduction number (R0) for COVID-19 in January were between 1.4 and 2.5,[351] but a subsequent analysis has concluded that it may be about 5.7 (with a 95-per-cent confidence interval of 3.8 to 8.9).[352]
Deaths
Further information: List of deaths due to coronavirus disease 2019Most people who contract COVID-19 recover. For those who do not, the time between the onset of symptoms and death ranges between 6 and 41 days, typically about 14 days.[358] As of 28 April 2020, approximately 213,000[5] deaths had been attributed to COVID-19. In China, as of 5 February, about 80 per cent of deaths were recorded in those aged over 60, and 75 per cent had pre-existing health conditions including cardiovascular diseases and diabetes.[359]
The first confirmed death was in Wuhan on 9 January 2020.[360] The first death outside China occurred on 1 February in the Philippines,[361] and the first death outside Asia was in France on 14 February.[362]
Official deaths from the COVID-19 generally refer to people who died after testing positive according to official protocols. This may ignore deaths of people who die without testing, e.g. at home or in nursing homes.[363] Conversely, deaths of people who had underlying conditions may lead to overcounting.[364] Comparison of statistics for deaths for all causes versus the seasonal average indicates excess mortality in many countries including most European countries, [365] [366] China,[367] the U.S.,[368] Iran,[369] Russia,[370] and Brazil.[371] In the worst affected areas, mortality has been several times higher than average. In New York City, deaths have been four times higher than average, in Paris twice as high, and in many European countries deaths have been on average 20 to 30 per cent higher than normal.[365]
Several measures are commonly used to quantify mortality.[372] These numbers vary by region and over time, and are influenced by the volume of testing, healthcare system quality, treatment options, time since initial outbreak, and population characteristics, such as age, sex, and overall health.[373] Some countries (like Belgium) include deaths from suspected cases of COVID-19, whether or not the person was tested, resulting in higher numbers when compared to countries that include only test-confirmed cases.[374]
The death-to-case ratio reflects the number of deaths attributed to COVID-19 divided by the number of diagnosed cases within a given time interval. Based on Johns Hopkins University statistics, the global death-to-case ratio is 6.9 per cent (213,824 deaths for 3,083,467 cases) as of 28 April 2020.[5] The number varies by region.[375]
Other measures include the case fatality rate (CFR), which reflects the percentage of diagnosed people who die from a disease, and the infection fatality rate (IFR), which reflects the percentage of infected (diagnosed and undiagnosed) who die from a disease. These statistics are not timebound and follow a specific population from infection through case resolution. Our World in Data states that as of 25 March 2020 the IFR cannot be accurately calculated.[376] The World Health Organization estimated the IFR at 0.37 per cent to 2.9 per cent.[377] The University of Oxford's Centre for Evidence-Based Medicine (CEBM) estimates a global CFR of 0.72 per cent and IFR of 0.1 per cent to 0.36 per cent.[378] According to CEBM, random antibody testing in Germany suggests an IFR of 0.37 per cent.[378]
Duration
The WHO said on 11 March 2020 the pandemic could be controlled.[7] The peak and ultimate duration of the outbreak are uncertain and may differ by location. Maciej Boni of Penn State University said, "Left unchecked, infectious outbreaks typically plateau and then start to decline when the disease runs out of available hosts. But it's almost impossible to make any sensible projection right now about when that will be".[381] The Chinese government's senior medical adviser Zhong Nanshan argued that "it could be over by June" if all countries can be mobilised to follow the WHO's advice on measures to stop the spread of the virus.[381] On 17 March, Adam Kucharski of the London School of Hygiene & Tropical Medicine said SARS‑CoV‑2 "is going to be circulating, potentially for a year or two".[382] According to the Imperial College study led by Neil Ferguson, physical distancing and other measures will be required "until a vaccine becomes available (potentially 18 months or more)".[383] William Schaffner of Vanderbilt University said, "I think it's unlikely that this coronavirus—because it's so readily transmissible—will disappear completely" and it "might turn into a seasonal disease, making a comeback every year". The virulence of the comeback would depend on herd immunity and the extent of mutation.[384]
Signs and symptoms
Main article: Coronavirus disease 2019Symptoms of COVID-19[385]
Symptoms of COVID-19 can be relatively non-specific and infected people may be asymptomatic. The two most common symptoms are fever (88 per cent) and dry cough (68 per cent). Less common symptoms include fatigue, respiratory sputum production (phlegm), loss of the sense of smell (initially estimated at 30 per cent[386] but later at only 15 per cent[387]), shortness of breath, muscle and joint pain, sore throat, headache, chills, vomiting, hemoptysis, and diarrhea.[388][18]
The WHO says approximately one person in five becomes seriously ill and has difficulty breathing.[8] The U.S. Centers for Disease Control and Prevention (CDC) lists emergency symptoms as difficulty breathing, persistent chest pain or pressure, sudden confusion, difficulty waking, and bluish face or lips; immediate medical attention is advised if these symptoms are present.[19]
Further development of the disease can lead to potentially fatal complications including pneumonia, acute respiratory distress syndrome, sepsis, septic shock, and kidney failure.[389]
Some of those infected may be asymptomatic, with no clinical symptoms but test results that confirm infection, so researchers have issued advice that those with close contact to confirmed infected people should be closely monitored and examined to rule out infection.[390] Chinese estimates of the asymptomatic ratio range from few to 44 per cent.[391] The usual incubation period (the time between infection and symptom onset) ranges from one to 14 days; it is most commonly five days.[392][8]
Cause
TransmissionFurther information: Fomite and Contact tracing
Respiratory droplets, produced during a sneeze

Some details about how the disease is spread are still being determined.[9] The disease is believed to be primarily spread during close contact and by small droplets produced during coughing, sneezing, or talking;[8][9][11] with close contact being within 1 to 2 metres (3 to 6 feet).[8][9] Both sputum and saliva can carry large viral loads.[393] Studies have found that an uncovered cough can lead to droplets travelling up to 4.5 metres (15 feet) to 11.4 metres (37 feet).[394][395][10] Some have proposed the virus may also be transmitted by small droplets that stay for more prolonged periods in the air, as may be generated during speech.[396]
These small droplets are also produced during breathing out, including when talking, although they usually fall to the ground or surfaces, as opposed to being infectious over large distances.[8][397] The droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs.[398] Some medical procedures such as intubation and cardiopulmonary resuscitation (CPR) may cause respiratory secretions to be aerosolised and thus result in airborne spread.[397] It may also spread when one touches a contaminated surface, including skin, and then touches their eyes, nose, or mouth.[8] While there are concerns it may spread by faeces, this risk is believed to be low.[8][9] The Government of China denied the possibility of faecal–oral transmission of SARS‑CoV‑2.[399]
The virus is most contagious during the first three days after onset of symptoms, although spread has been reported before symptoms appear and in later stages of the disease.[9][400][401] There have been reports of transmission during the three days preceding symptoms.[401] During this period, people have also tested positive for the disease, suggesting transmission is possible before symptoms develop.[400][401][402] Laboratory-confirmed asymptomatic cases have been detected.[401] The European Centre for Disease Prevention and Control (ECDC) says while it is not entirely clear how easily the disease spreads, one person generally infects two to three others.[11]
The virus survives for hours to days on surfaces.[11][403] Specifically, the virus was found to be detectable for up to three days on plastic (polypropylene) and 304 stainless steel, for one day on cardboard, and for up to four hours on copper.[14] This, however, varies based on the humidity and temperature.[404]
Pets and other animals have tested positive for COVID-19.[405] There is no evidence animals can pass the virus on to humans,[406] though British authorities advise washing one's hands after contact with animals, like after contact with other potentially contaminated surfaces.[407][408]
Virology
Main article: Severe acute respiratory syndrome coronavirus 2

Illustration of SARSr‑CoV virion
Severe acute respiratory syndrome coronavirus 2 (SARS‑CoV‑2) is a novel virus, first isolated from three people with pneumonia connected to the cluster of acute respiratory illness cases in Wuhan.[328] All features of the novel SARS‑CoV‑2 virus occur in related coronaviruses in nature.[409]
SARS‑CoV‑2 is closely related to SARS‑CoV, and is thought to have a zoonotic origin.[325] SARS‑CoV‑2 genetically clusters with the genus Betacoronavirus, and is 96 per cent identical at the whole genome level to other bat coronavirus samples[388] and 92 per cent identical to pangolin coronavirus.[410]
Diagnosis
Main article: COVID-19 testing
Demonstration of a swab for COVID-19 testing
COVID-19 can be provisionally diagnosed on the basis of symptoms and confirmed using reverse transcription polymerase chain reaction (rRT-PCR) testing of infected secretions or CT imaging of the chest.[411][412]
Viral testing
The standard test for current infection with SARS-CoV-2 uses RNA testing of respiratory secretions collected using a nasopharyngeal swab, though it is possible to test other samples. This test uses real-time rRT-PCR which detects presence of viral RNA fragments.[413]
A number of laboratories and companies are developing serological tests, which detect antibodies produced by the body in response to infection.[414] As of 6 April 2020, none of these has been proved sufficiently accurate to be approved for widespread use.[415]
Imaging
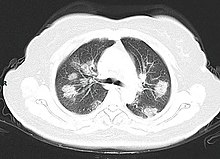
A CT scan of the chest of a person with COVID‑19. It shows light patches in the lungs.
Characteristic imaging features on chest radiographs and computed tomography (CT) of people who are symptomatic include asymmetric peripheral ground-glass opacities without pleural effusions.[416] The Italian Radiological Society is compiling an international online database of imaging findings for confirmed cases.[417] Due to overlap with other infections such as adenovirus, imaging without confirmation by rRT-PCR is of limited specificity in identifying COVID-19.[416] A large study in China compared chest CT results to PCR and demonstrated that though imaging is less specific for the infection, it is faster and more sensitive.[412]
Prevention
Further information: Workplace hazard controls for COVID-19, Pandemic prevention, and Preparation to COVID-19
Infographic by the United States CDC, describing how to stop the spread of germs
Strategies for preventing transmission of the disease include maintaining overall good personal hygiene, washing hands, avoiding touching the eyes, nose, or mouth with unwashed hands, and coughing or sneezing into a tissue and putting the tissue directly into a waste container. Those who may already have the infection have been advised to wear a surgical mask in public.[418][419] Physical distancing measures are also recommended to prevent transmission.[420][421] Health care providers taking care of someone who may be infected are recommended to use standard precautions, contact precautions, and eye protection.[422]
Many governments have restricted or advised against all non-essential travel to and from countries and areas affected by the outbreak.[423] However, the virus is already spreading within communities in large parts of the world, with many not knowing where or how they were infected.[398]
Misconceptions are circulating about how to prevent infection; for example, rinsing the nose and gargling with mouthwash are not effective.[424] There is no COVID-19 vaccine, though many organisations are working to develop one.[425]
Hand washing
Main article: Hand washing
Hand washing is recommended to prevent the spread of the disease. The CDC recommends that people wash hands often with soap and water for at least twenty seconds, especially after going to the toilet or when hands are visibly dirty; before eating; and after blowing one's nose, coughing, or sneezing. This is because outside the human body, the virus is killed by household soap, which bursts its protective bubble.[24] CDC further recommended using an alcohol-based hand sanitiser with at least 60 per cent alcohol by volume when soap and water are not readily available.[418] The WHO advises people to avoid touching the eyes, nose, or mouth with unwashed hands.[419][426]
Surface cleaning
Surfaces may be decontaminated with a number of solutions (within one minute of exposure to the disinfectant for a stainless steel surface), including 62–71 per cent ethanol, 50–100 per cent isopropanol, 0.1 per cent sodium hypochlorite, 0.5 per cent hydrogen peroxide, and 0.2–7.5 per cent povidone-iodine. Other solutions, such as benzalkonium chloride and chlorhexidine gluconate, are less effective.[427] The CDC recommends that if a COVID case is suspected or confirmed at a facility such as an office or day care, all areas such as offices, bathrooms, common areas, shared electronic equipment like tablets, touch screens, keyboards, remote controls, and ATM machines used by the ill persons, should be disinfected.[428]
Face masks and respiratory hygiene
Main article: Face masks during the 2019–20 coronavirus pandemic
Taiwan President Tsai Ing-wen wearing a mask
Health organisations recommended that people cover the mouth and nose with a bent elbow or a tissue when coughing or sneezing, and disposing of any tissue immediately.[419] Surgical masks are recommended for those who may be infected, as wearing a mask can limit the volume and travel distance of expiratory droplets dispersed when talking, sneezing, and coughing.[429] The WHO has issued instructions on when and how to use masks.[429]
Masks have also been recommended for use by those taking care of someone who may have the disease.[429] The WHO has recommended healthy people wear masks only if they are at high risk, such as those who are caring for a person with COVID-19.[429] China and the United States, among other countries, have encouraged the use of face masks or cloth face coverings more generally by members of the public to limit the spread of the virus by asymptomatic individuals as a precautionary principle.[430][431][432] Several national and local governments have made wearing masks mandatory.[431][433][434][435] Varying recommendations for wearing masks have been a subject of debate.[436]
Social distancing
Main article: Social distancing measures related to the 2019–20 coronavirus pandemic
Physical distancing in Toronto, with limited number of customers allowed inside the store
Social distancing (also known as physical distancing) includes infection control actions intended to slow the spread of disease by minimising close contact between individuals. Methods include quarantines; travel restrictions; and the closing of schools, workplaces, stadiums, theatres, or shopping centres. Individuals may apply social distancing methods by staying at home, limiting travel, avoiding crowded areas, using no-contact greetings, and physically distancing themselves from others.[419][437] Many governments are now mandating or recommending social distancing in regions affected by the outbreak.[438][439] The maximum gathering size recommended by U.S. government bodies and health organisations was swiftly reduced from 250 people (if there was no known COVID-19 spread in a region) to 50 people, and later to 10.[440] On 22 March 2020, Germany banned public gatherings of more than two people.[441] A Cochrane review found that early quarantine with other public health measures are effective in limiting the pandemic, but the best manner of adopting and relaxing policies are uncertain, as local conditions vary.[442]
The pandemic in Peru resulted in curfews enforced by the Peruvian Armed Forces.
Older adults and those with underlying medical conditions such as diabetes, heart disease, respiratory disease, hypertension, and compromised immune systems face increased risk of serious illness and complications and have been advised by the CDC to stay home as much as possible in areas of community outbreak.[443][444]
In late March 2020, the WHO and other health bodies began to replace the use of the term "social distancing" with "physical distancing", to clarify that the aim is to reduce physical contact while maintaining social connections, either virtually or at a distance. The use of the term "social distancing" had led to implications that people should engage in complete social isolation, rather than encouraging them to stay in contact with others through alternative means.[445][446]
Some authorities have issued sexual health guidelines for use during the pandemic. These include recommendations to have sex only with someone you live with, and who does not have the virus or symptoms of the virus.[447][448]
Self-isolation
Transmission of COVID-19 depends on many factors, most obviously physical distance.
Self-isolation at home has been recommended for those diagnosed with COVID-19 and those who suspect they have been infected. Health agencies have issued detailed instructions for proper self-isolation.[449][450]
Many governments have mandated or recommended self-quarantine for entire populations living in affected areas.[451][452] The strongest self-quarantine instructions have been issued to those in high risk groups. Those who may have been exposed to someone with COVID-19 and those who have recently travelled to a country or region with widespread transmission have been advised to self-quarantine for 14 days from the time of last possible exposure.[8][21][453]
Management
Further information: Coronavirus disease 2019 § Management, and Pandemic § ManagementContainment and mitigation
Further information: Flatten the curve

Goals of mitigation include delaying and reducing peak burden on healthcare (flattening the curve) and lessening overall cases and health impact.[454][455] Moreover, progressively greater increases in healthcare capacity (raising the line) such as by increasing bed count, personnel, and equipment, helps to meet increased demand.[456]
Mitigation attempts that are inadequate in strictness or duration—such as premature relaxation of distancing rules or stay-at-home orders—can allow a resurgence after the initial surge and mitigation.[454][457]
Strategies in the control of an outbreak are containment or suppression, and mitigation. Containment is undertaken in the early stages of the outbreak and aims to trace and isolate those infected as well as introduce other measures of infection control and vaccinations to stop the disease from spreading to the rest of the population. When it is no longer possible to contain the spread of the disease, efforts then move to the mitigation stage: measures are taken to slow the spread and mitigate its effects on the healthcare system and society. A combination of both containment and mitigation measures may be undertaken at the same time.[458] Suppression requires more extreme measures so as to reverse the pandemic by reducing the basic reproduction number to less than 1.[383]
Part of managing an infectious disease outbreak is trying to delay and decrease the epidemic peak, known as flattening the epidemic curve.[454] This decreases the risk of health services being overwhelmed and provides more time for vaccines and treatments to be developed.[454] Non-pharmaceutical interventions that may manage the outbreak include personal preventive measures, such as hand hygiene, wearing face masks, and self-quarantine; community measures aimed at physical distancing such as closing schools and cancelling mass gathering events; community engagement to encourage acceptance and participation in such interventions; as well as environmental measures such surface cleaning.[459]
More drastic actions aimed at containing the outbreak were taken in China once the severity of the outbreak became apparent, such as quarantining entire cities and imposing strict travel bans.[460] Other countries also adopted a variety of measures aimed at limiting the spread of the virus. South Korea introduced mass screening and localised quarantines, and issued alerts on the movements of infected individuals. Singapore provided financial support for those infected who quarantined themselves and imposed large fines for those who failed to do so. Taiwan increased face mask production and penalised hoarding of medical supplies.[461]
Simulations for Great Britain and the United States show that mitigation (slowing but not stopping epidemic spread) and suppression (reversing epidemic growth) have major challenges. Optimal mitigation policies might reduce peak healthcare demand by two-thirds and deaths by half, but still result in hundreds of thousands of deaths and overwhelmed health systems. Suppression can be preferred but needs to be maintained for as long as the virus is circulating in the human population (or until a vaccine becomes available), as transmission otherwise quickly rebounds when measures are relaxed. Long-term intervention to suppress the pandemic has considerable social and economic costs.[383]
Contact tracing
See also: Coronavirus disease 2019 § Information technology
Contact tracing is an important method for health authorities to determine the source of an infection and to prevent further transmission.[462] The use of location data from mobile phones by governments for this purpose has prompted privacy concerns, with Amnesty International and more than a hundred other organisations issuing a statement calling for limits on this kind of surveillance.[463]
Various mobile apps have been implemented or proposed for voluntary use, and as of 7 April 2020 more than a dozen expert groups were working on privacy-friendly solutions such as using Bluetooth to log a user's proximity to other cellphones.[463] Users could then receive a message if they've been in close contact with someone who has subsequently tested positive for COVID-19.[463]
On 10 April 2020 Google and Apple, jointly announced an initiative for privacy-preserving contact tracing based on Bluetooth technology and cryptography.[464][465] The system is intended to allow governments to create official privacy-preserving coronavirus tracking apps, with the eventual goal of integration of this functionality directly into the iOS and Android mobile platforms.[466]
Health care
Further information: Flatten the curve, list of countries by hospital beds, and Shortages related to the 2019–20 coronavirus pandemic

An army-constructed field hospital outside Östra sjukhuset (Eastern hospital) in Gothenburg, Sweden, contains temporary intensive care units for COVID-19 patients.
Increasing capacity and adapting healthcare for the needs of COVID-19 patients is described by the WHO as a fundamental outbreak response measure.[467] The ECDC and the European regional office of the WHO have issued guidelines for hospitals and primary healthcare services for shifting of resources at multiple levels, including focusing laboratory services towards COVID-19 testing, cancelling elective procedures whenever possible, separating and isolating COVID-19 positive patients, and increasing intensive care capabilities by training personnel and increasing the number of available ventilators and beds.[467][468]
Due to capacity limitations in the standard supply chains, some manufacturers are 3D printing healthcare material such as nasal swabs and ventilator parts.[469][470] In one example, when an Italian hospital urgently required a ventilator valve, and the supplier was unable to deliver in the timescale required, a local startup risked legal threats due to alleged patent infringement and reverse-engineered and printed the required hundred valves overnight.[471][472][473] On 23 April 2020, NASA reported building, in 37 days a ventilator which is currently undergoing further testing. NASA is seeking fast-track approval.[474][475]
Treatment
There are no specific antiviral medications approved for COVID-19, but development efforts are underway, including testing of existing medications. Taking over-the-counter cold medications,[476] drinking fluids, and resting may help alleviate symptoms.[418] Depending on the severity, oxygen therapy, intravenous fluids, and breathing support may be required.[477] The use of steroids may worsen outcomes.[478] Several compounds which were previously approved for treatment of other viral diseases are being investigated for use in treating COVID-19.[479]










Comments
Post a Comment